James' Story
James Miller, 38, enjoys hunting, fishing and spending time with his wife, Danielle, and his 15-year-old son. One morning as Danielle was saying goodbye and heading out the door, she realized James couldn’t speak. She immediately called an ambulance and he was taken to Slidell Memorial Hospital in Louisiana. While in the Emergency Department, doctors discovered a brain bleed, called a hemorrhagic stroke, on the left side of James’ brain due to an aneurysm rupture.
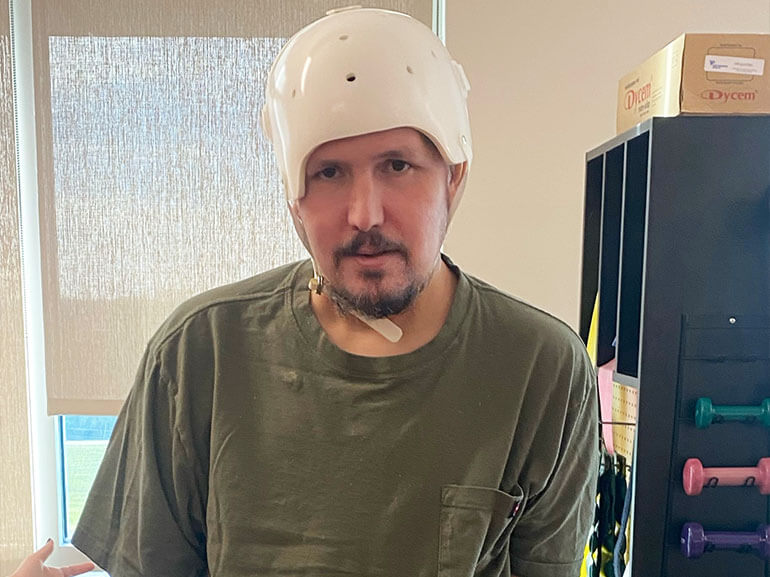
James was then transferred to Ochsner Main Campus for additional tests and treatment. Cardiac tests further revealed an infection and irregular growths in his heart. Complications continued, including a COVID-19 infection and a second stroke while he was in the hospital. Due to the swelling on James’ brain, doctors performed a partial craniectomy, in which they removed a portion of the skull to relieve pressure on the brain from swelling. Because of this, James had to wear a helmet at all times when out of bed throughout his recovery journey.
Once medically stable, James was transferred to post-acute care, then to a brain-injury specific facility. While there, he continued to have difficulty swallowing and ended up inhaling food into his airway, called aspiration, which can cause infection. After this incident, he was transferred back to Ochsner Main Campus, then admitted to Ochsner Rehabilitation Hospital to continue his recovery journey.
When he first arrived, James was unable to eat and required assistance with all levels of self-care. Additionally, it took two people to transfer him from his bed to the wheelchair as he wasn’t able to use his right arm. James was also unable to communicate.
He immediately started intense occupational therapy that focused on self-care skills, functional mobility and use of his right arm. His therapists performed activities of daily living training on a weekly basis which focused on dressing techniques. They also worked with James on transfer and balance training. Additionally, time was spent reconnecting James’ brain and body functioning through electrical stimulation therapy to improve range of motion and the overall function in his right arm.
James and Danielle participated in family training to prepare for his return home. James made significant improvement with his activities of daily living from initially requiring total assistance to only needing minimal assistance with some tasks.
Simultaneously, physical therapy focused on increasing James’ muscle strength and coordination in order to help him regain his mobility. When admitted to Ochsner Rehabilitation Hospital, James required maximal assistance to stand and get in and out of bed. He was only able to walk three feet with significant assistance to shift his weight and move his right leg. James’s impairments included: right-sided weakness, impaired posture, decreased muscle tone in his right leg, decreased endurance, impaired balance, communication deficits and cognitive challenges. His physical therapist focused on improving James’s ability to stand using several bodyweight support systems (LiteGait and Tollos) to improve his ability to move his right leg, shift his weight and walk longer distances. James required the use of an ankle foot orthotic on his right foot to improve his foot clearance and the quality of his walking. By the time James discharged, he was able to walk nearly 150 feet on his own with a one-sided walker, called a hemiwalker, and an ankle foot orthotic. He was also able to stand and transfer and propel his wheelchair without assistance.
After the stroke, James experienced a language disorder known as aphasia. Aphasia refers to a communication disorder that results from damage to the language control center in the brain. Due to the severity of James’s aphasia, he could not verbally express himself and had substantial difficulty comprehending basic information. James’s speech therapist used an aid called an AAC (augmentative and alternative communication) board to assist James in communicating his basic wants and needs. James’s AAC board consisted of a few choices (yes/no, I don’t know and a pain scale) to avoid overstimulation. To further improve comprehension, his speech therapist worked with James on following basic directions. By the end of his stay, James was able to comprehend basic information and express his wants and needs.
Another challenge James faced during rehabilitation was dysphagia. Dysphagia refers to difficulty swallowing due to weakness of the swallowing muscles. When James first admitted to Ochsner Rehabilitation Hospital, he received all nutrition, hydration and medication through a feeding tube because his swallowing muscles were weak, compromising his airway. To objectively assess the function of James’ swallow, he participated in an instrumental swallowing assessment known as FEES. FEES stands for Fiberoptic Endoscopic Evaluation of Swallowing, in which a tube with a camera on the end is inserted into the nasal passage. Once through the nasal passage, the camera gives a clear view of the patient’s throat and swallow functioning while the patient eats and drinks various consistencies. If food or liquid is seen entering the airway, the patient is at risk of developing aspiration pneumonia. The initial FEES assessment revealed that James was at high risk of aspiration. Over the next couple weeks, James’ therapist continued to assess his ability to tolerate various food and drink textures safely. A follow up evaluation showed his swallowing function had improved significantly, and he was cleared to eat soft, solid foods and drink regular liquids.
After 28 days at Ochsner Rehabilitation Hospital, James was ready to go home. He was very excited to see his dog, Scooby, and hang out with his son. He plans to continue rebuilding his strength through outpatient therapy services.
For other patients facing a long recovery road, James shares: “Have a strong will and push through the hard days.”